-
-
Access Free Student Software
Ansys empowers the next generation of engineers
Students get free access to world-class simulation software.
-
Connect with Ansys Now!
Design your future
Connect with Ansys to explore how simulation can power your next breakthrough.
Countries & Regions
Free Trials
Products & Services
Learn
About
Back
Products & Services
Back
Learn
Ansys empowers the next generation of engineers
Students get free access to world-class simulation software.
Back
About
Design your future
Connect with Ansys to explore how simulation can power your next breakthrough.
Free Trials

Boston Children’s Hospital has led the way in life-changing pediatric innovation since its founding in 1869. Today, Boston Children’s remains committed to pursuing treatments for some of the most challenging diseases and conditions through extensive research and integration of innovative technologies.
At Boston Children’s Hospital, multidisciplinary collaboration lies at the heart of innovation. Clinicians, engineers, and scientists work side by side to translate fundamental discoveries into practical, patient-centered solutions. By integrating clinical insight with advanced engineering, data science, and computational modeling, teams can identify unmet clinical needs, rapidly prototype new technologies, and rigorously evaluate their impact. This collaborative ecosystem enables the seamless translation of research innovations from bench to bedside, ensuring that emerging technologies directly enhance patient care and clinical decision-making.
This multidisciplinary collaborative approach enables Boston Children’s to incorporate engineering solutions to tackle challenges in pediatric care, such as optimizing blood flow during surgery or providing a quantitative understanding of blood flow in extracorporeal membrane oxygenation (ECMO) circuits. Let's explore how Boston Children's is transforming how treatments for patients with complex heart conditions are planned and executed by combining simulation technology with clinical expertise.

A membrane oxygenator, also known as an artificial lung, is used in extracorporeal membrane oxygenation (ECMO) to temporarily draw blood from the body to allow artificial oxygenation of the red blood cells and removal of carbon dioxide.
CFD: The Lifeblood of Cardiac Care
How often do you think about how blood flows through your body? Probably not very often. Unless you have a known blood or cardiac disorder, it’s easy to assume that your blood circulates without any issues. In practice, the dynamics of blood flow through the vascular system, referred to as hemodynamics, varies substantially across individuals. For children born with congenital heart defects (CHD), blood flow is often abnormal and requires corrective surgery. A critical measure of surgical success, and of the child’s long-term health, is whether adequate, balanced blood flow and physiologic pressures are delivered post-operatively to each of the body’s vital organs.
“Flow efficiency is paramount in congenital heart defect patients,” says Vijay Govindarajan, Ph.D., assistant professor of surgery at Harvard Medical School and Boston Children’s, who also serves as scientific director of flow simulation and multiphysics modeling at Boston Children's Cardiovascular 3D Modeling and Simulation Program. “We use computational fluid dynamics, or CFD, to compute the existing flow efficiency, then perform virtual surgical scenarios to determine the best surgical approach that delivers the most optimal hemodynamics for the patients using CFD simulations.”
By modeling the cardiovascular system and simulating adjustments to procedures, CFD software helps identify the most efficient surgical pathways for complex cardiac cases. Govindarajan and team use Ansys Fluent fluid simulation software to predict how changes in flow dynamics might affect overall circulation, which enables surgeons to refine their strategies before operating. Fluent software not only helps quantify flow efficiency and assess areas of high dissipation within the region of interest, it also helps predict other hemodynamic factors critical for surgical success. By analyzing these variables in a virtual environment, the surgical team can anticipate challenges and make data-informed adjustments to their plans, ultimately reducing the risk of complications during the procedure.
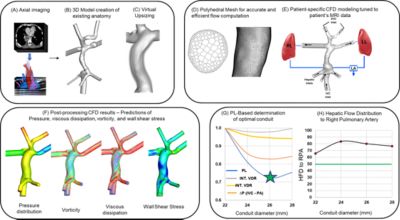
An illustration of the computational workflow for performing virtual upsizing of Fontan and subsequent analysis. The Fontan procedure is an operation to improve circulation in patients with only one working ventricle.
“Blood flow itself is highly sensitive to the geometry of the anatomy,” explains Govindarajan. “So a small change in the geometry can have a significant impact on the flow. And since patients with congenital heart defects have highly individualized anatomies, a surgical approach that works well for one patient may not be effective for another.”
In addition to Fluent software, Govindarajan and the modeling team use Ansys SpaceClaim 3D computer-aided design (CAD) modeling software and Ansys ICEM CFD mesh generation capabilities to create detailed models of individual patients and mesh them for high-fidelity flow simulations. This level of precision helps refine surgical techniques to determine strategies best suited to the patient’s specific needs, which reduces the likelihood of complications during procedures. Additionally, patient-specific modeling helps surgeons anticipate potential complications associated with unique anatomical structures or flow characteristics. Together, these factors help reduce potential short- and long-term complications, improving surgical effectiveness.
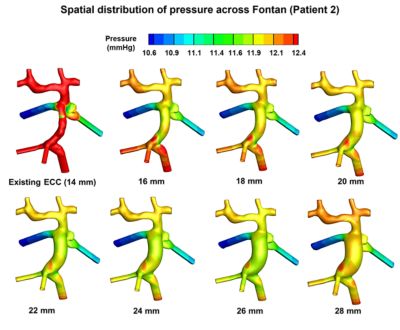
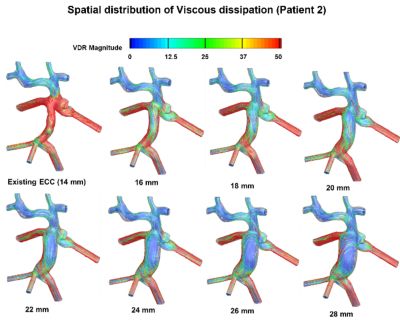
Left: A model prediction of the spatial distribution of pressure across Fontan for patient two. Predictions show that pressure distribution across Fontan decreases as Fontan conduit size is virtually upsized to improve hemodynamics. Right: A model prediction of the spatial distribution of viscous dissipation rate (VDR) across Fontan for patient two. VDR decreases across Fontan as Fontan conduit size is virtually upsized, making the flow efficient.
“Each patient has a unique anatomy that necessitates significant personalization, and that is where the simulation tools are hugely helpful,” says Govindarajan.
Modeling Hemodynamics in Pediatric ECMO Circuits
“We initiated the development of a new CFD framework tailored specifically for ECMO, following the development of our CFD-based surgical planning workflow for patients born with single ventricle heart defects,” says Govindarajan. “Because many of the hemodynamic challenges faced in cardiac surgery, such as blood flow inefficiency, flow stasis, thrombosis, and shear-related blood damage, also arise in ECMO, we were motivated to develop a dedicated modeling approach to better understand and optimize ECMO performance.”
ECMO circuits are a series of pumps, chambers, and tubes that temporarily support the function of the heart and lungs of critically ill patients, specifically those with advanced heart failure or waiting for a transplant. ECMO circuits pump blood out of the body into an oxygenator chamber to remove carbon dioxide and reoxygenate the blood, then pump it back through the body. While it might seem like the challenges between surgery and mechanical pumps are worlds apart, they carry a significant common issue, namely, blood clots also known as thrombosis.
A delicate balance must be achieved because blood can clot excessively (thrombosis) or bleed (hemorrhage), and anatomical abnormalities, patient-specific anomalies, or the presence of medical devices can further accelerate clot formation which is undesirable when patients are managed under ECMO. Blood clots can occur anywhere in the ECMO circuit where there are flow irregularities, such as around tubing connectors or within an ECMO pump. By integrating Fluent software, Govindarajan and the research team created highly detailed models of these circuits, providing essential insights into how blood moves under many different pump speeds. The team can predict and quantify any flow irregularities, such as flow stasis, excessive turbulence, and shear stresses that could compromise circuit performance and impact patient care.
Using this computational modeling framework and its quantitative findings, clinicians and engineers can refine the design of ECMO components, making them safer and more effective for pediatric patients. Such CFD modeling framework enables ongoing advancements in customizing ECMO systems, ensuring they are better aligned with the unique physiological conditions of each patient. Such precise analysis can not only aid in preventing complications but also support the development of strategies to enhance the reliability and safety of ECMO therapies.
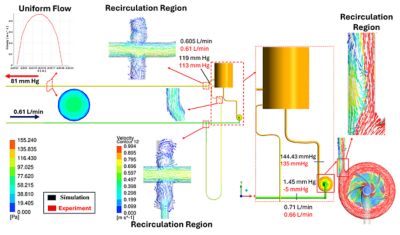
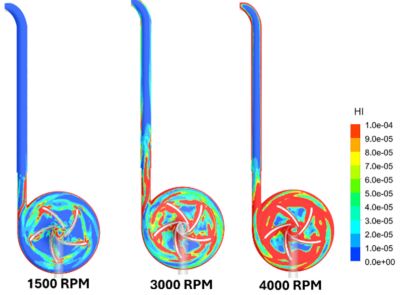
Left: Flow characteristics in an ECMO circuit, highlighting areas of flow separation and recirculation at different regions. A sudden expansion at the connector region can induce flow separation and localized stasis. Further downstream, a sudden expansion at the connector outlet can lead to additional recirculation near the walls. Right: Contours of the hemolysis index, which quantifies blood cell damage, illustrate the spatial distribution of blood damage along the pump and downstream tubing toward the membrane lung across different pump speeds. Regions of elevated hemolysis originate near the pump and propagate downstream through the circuit, with overall hemolytic stress increasing at higher rotational speeds.
Using Personalized Predictive Models for Better Care
Simulation software is instrumental in creating predictive models that offer critical insights into patient-specific scenarios. These models enable clinicians to simulate surgical options and identify the most effective approach tailored to each individual. With ECMO, in which the interplay between blood flow and circuit performance is highly sensitive, this ability to anticipate outcomes is highly beneficial.
Predictive modeling gives researchers the ability to quantitatively assess how blood flow patterns influence the effectiveness of an ECMO circuit. This information can help fine-tune treatment strategies, minimizing potential complications such as clot formation or inefficient oxygenation.
By simulating real-world scenarios, Boston Children’s is able to gain the knowledge needed to refine medical and surgical protocols. Computational modeling and simulation help doctors make better decisions surrounding patient care, ensuring that interventions take the unique needs of each patient into account. The enhanced precision that simulation offers can help reduce recovery times and improve overall care, making pediatric treatment safer and more effective.
Learn more about how Ansys can help with your cardiovascular simulation needs.
Just for you. We have some additional resources you may enjoy.
“Each patient has a unique anatomy that necessitates significant personalization, and that is where the simulation tools are hugely helpful.”
— Vijay Govindarajan, Ph.D., assistant professor of surgery at Harvard Medical School and Boston Children’s Hospital and scientific director of flow simulation and multiphysics modeling at Boston Children’s Hospital Cardiovascular 3D Modeling and Simulation Program
The Advantage Blog
The Ansys Advantage blog, featuring contributions from Ansys and other technology experts, keeps you updated on how Ansys simulation is powering innovation that drives human advancement.